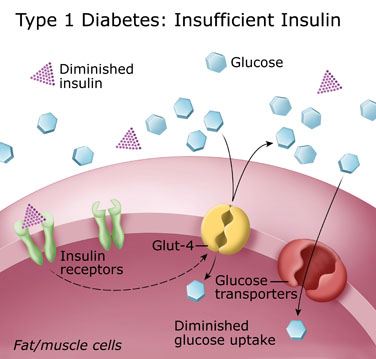
Type 1 diabetes is caused by a loss or malfunction of the insulin producing cells, called pancreatic beta cells. Damage to beta cells results in an absence or insufficient production of insulin produced by the body. Most cases of type 1 diabetes have an autoimmune basis, and the immune system mistakenly attacks and destroys beta cells. Since insulin is necessary to sustain life, the missing insulin has to be replaced. The replacement insulin is administered by injection using a syringe or an insulin pump, which delivers the insulin under the skin.
Basic facts about type 1 diabetes
Type 1 diabetes accounts for about 5-10% of diabetes worldwide.
- It is diagnosed in every ethnic group, but is most frequent in individuals of European ancestry.
- While type 1 diabetes is commonly diagnosed during adolescence and early adulthood, it can occur at any age. Older people who develop type 1 diabetes are often misdiagnosed as having Type 2 diabetes.
- Most people first diagnosed with type 1 diabetes are lean.
- 85-90% will have no known family history of the disease.
- There are many theories about what causes type 1 diabetes. Autoimmune disease, viral infection, genetic disposition, and environmental factors may all play a role.
- There is a hereditary component to type 1 diabetes; however, it is still difficult to predict who will develop it. Among identical twins (who presumably have the same genetic and environmental risk), it is traditionally reported that only about 40% will both have the disease. Recent research suggests that the number may be much higher.
- Markers in your blood and the presence of certain gene types, coupled with test results, can help predict who might develop diabetes.
- Diabetes researchers are seeking ways to identify both high-risk individuals and ways to protect them. Read more about Type 1 Research.
Sub categories of Type 1 diabetes
There are 2 sub categories of Type 1 diabetes:
- Type 1a including Latent Autoimmune Diabetes of Adults (LADA)
- Type 1b
You have Type 1a if:
Your immune system is so overactive that it is destroying normal beta cell tissue. The telltale signs of this destruction are detectable by a laboratory blood test. The test looks for markers. The list of markers includes glutamic acid decarboxylase antibodies (GADA), islet cell antibodies to membranous tyrosine phosphatase (ICA-512), islet cell antibodies (ICA), and insulin auto antibodies (IAA).
Some adults have a slowly progressive autoimmune destruction of their beta cells referred to as Latent Autoimmune Diabetes of Adults or LADA. Sometimes this is also known as diabetes type 1 ½. Individuals with LADA may be treated for years with diet and pills, and often are misdiagnosed as having Type 2 diabetes. Ultimately insulin replacement therapy is necessary to control the blood sugar. A diagnosis is made by confirming the presence of antibody markers.
You have Type 1b if:
You meet two criteria: the first, if there is no evidence in your blood that your immune system is attacking beta cells and the second, if you have alternating cycles where you need and then don’t need insulin replacement. This form of the disease is unusual and most often diagnosed in those of African or Asian heritage.
Self-assessment Quiz
Self assessment quizzes are available for topics covered in this website. To find out how much you have learned about Facts about Diabetes, take our self assessment quiz when you have completed this section. The quiz is multiple choice. Please choose the single best answer to each question. At the end of the quiz, your score will display. If your score is over 70% correct, you are doing very well. If your score is less than 70%, you can return to this section and review the information.