Glucagon:
Glucagon, made by islet cells (alpha cells) in the pancreas, controls the production of glucose and another fuel, ketones, in the liver.
Glucagon is released overnight and between meals and is important in maintaining the body’s sugar and fuel balance. It signals the liver to break down its starch or glycogen stores and helps to form new glucose units and ketone units from other substances. It also promotes the breakdown of fat in fat cells.
In contrast, after a meal, when sugar from the ingested food rushes into your bloodstream, your liver doesn’t need to make sugar. The consequence? Glucagon levels fall.
Unfortunately, in individuals with diabetes, the opposite occurs. While eating, their glucagon levels rise, which causes blood sugar levels to rise after the meal.
WITH DIABETES, GLUCAGON LEVELS ARE TOO HIGH AT MEALTIMES
GLP-1 (glucagon-like peptide-1), GIP (glucose-dependent insulinotropic polypeptide) and amylin:
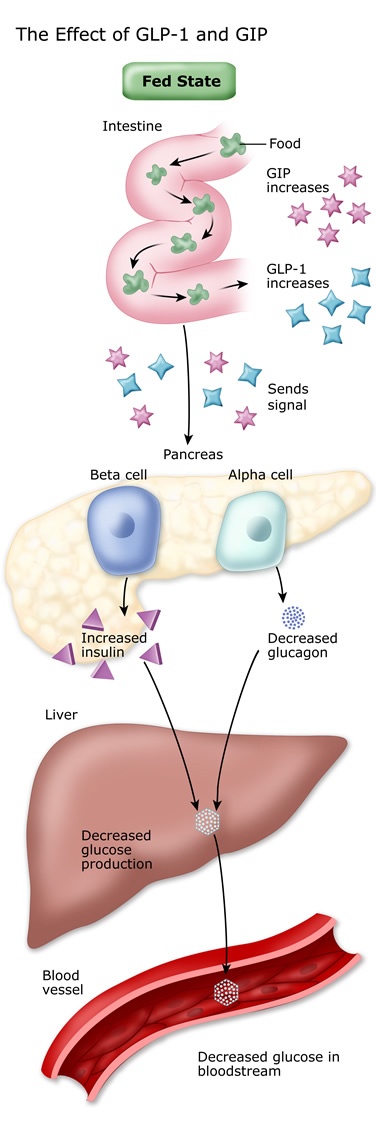
GLP-1 (glucagon-like peptide-1), GIP (glucose-dependent insulinotropic polypeptide) and amylin are other hormones that also regulate mealtime insulin. GLP-1 and GIP are incretin hormones. When released from your gut, they signal the beta cells to increase their insulin secretion and, at the same time, decrease the alpha cells’ release of glucagon. GLP-1 also slows down the rate at which food empties from your stomach, and it acts on the brain to make you feel full and satisfied.
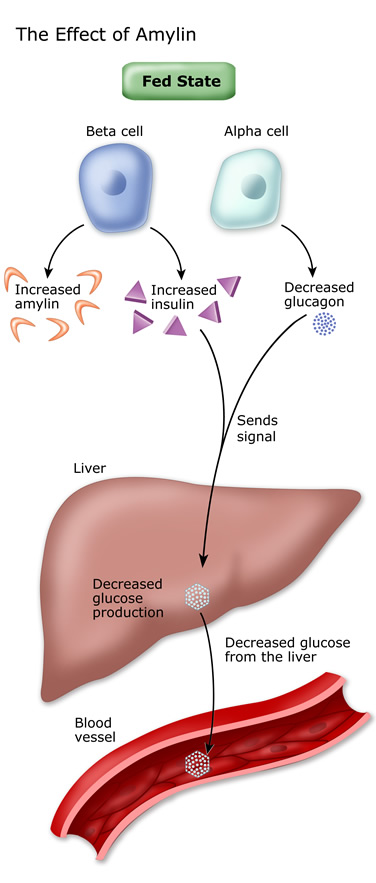
Amylin:
Amylin is released along with insulin from beta cells. It has much the same effect as GLP-1. It decreases glucagon levels, slows the rate at which food empties from your stomach, and makes your brain feel that you have eaten a full and satisfying meal. A fall in glucagon decreases the liver’s glucose production.
The overall effect of these hormones is to reduce the production of sugar by the liver during a meal to prevent it from getting too high.
People with type 2 diabetes have sub-normal amounts of GIP, and their beta cells don’t respond properly to GLP-1. This may explain why glucagon levels are not suppressed during a meal.
The good news is that synthetic versions of GLP-1 and amylin are now available as medicines to control post-meal glucagon and blood sugar in individuals with type 2 diabetes.
Epinephrine, cortisol, and growth hormone:
Epinephrine, cortisol, and growth hormone are other hormones that help maintain blood sugar levels. They, along with glucagon (see above) are called “stress” or “gluco-counter-regulatory” hormones – which means they make the blood sugar rise.
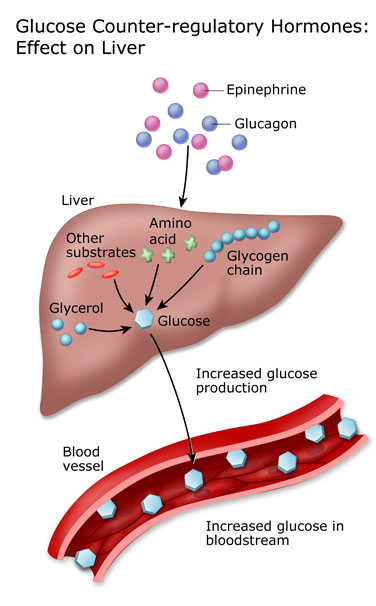
Epinephrine (adrenaline) is released from nerve endings and the adrenals, and acts directly on the liver to promote sugar production (via glycogenolysis). Epinephrine also promotes the breakdown and release of fat nutrients that travel to the liver and that are converted into sugar and ketones.
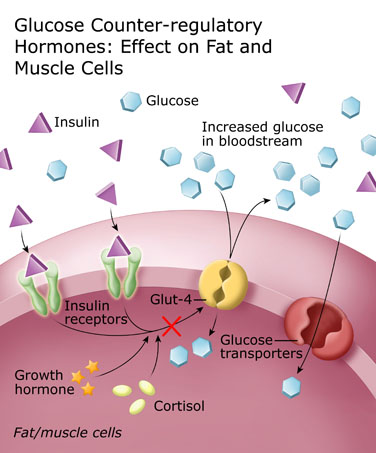
Cortisol is a steroid hormone also secreted from the adrenal gland. It makes fat and muscle cells resistant to the action of insulin, and enhances the production of glucose by the liver. Under normal circumstances, cortisol counterbalances the action of insulin. Under stress or if a synthetic cortisol is given as a medication (such as with prednisone therapy or cortisone injection), cortisol levels become elevated and you become insulin resistant. When you have Type 2 diabetes, this means your may need to take more medication or insulin to keep your blood sugar under control.
Growth Hormone is released from the pituitary, which is a part of the brain. Like cortisol, growth hormone counterbalances the effect of insulin on muscle and fat cells. High levels of growth hormone cause resistance to the action of insulin.
Self-assessment Quiz
Self assessment quizzes are available for topics covered in this website. To find out how much you have learned about Facts about Diabetes, take our self assessment quiz when you have completed this section. The quiz is multiple choice. Please choose the single best answer to each question. At the end of the quiz, your score will display. If your score is over 70% correct, you are doing very well. If your score is less than 70%, you can return to this section and review the information.
